All of us have had the unfortunate experience of dealing with pain at some point in our lives, but what is pain, and what causes it?
Pain is an unpleasant sensory and emotional response that signals damage or potential harm to the body. Each person’s experience of pain is unique and influenced by different biological, psychological, and social factors.
Short-term acute pain, long-term chronic pain, and recurrent pain can all cause significant distress. In some cases, the root cause of pain can be obvious, such as an injury, but pain can also be hard to identify, treat, and manage.
Pain signals are carried to the brain via the spinal cord and specialised nerve fibres. The brain interprets these signals and responds by triggering reactions and emotional responses. This complex network can sometimes go wrong, however, leading to persistent pain problems.
It is estimated that nearly 21% of US adults live with chronic pain, and more than a quarter of the UK population. Health services are often not designed to deal with complex pain conditions, making pain one of the most challenging issues for patients and doctors.
Chronic pain can have a significant impact on a person’s quality of life and their ability to conduct normal daily tasks. Understanding the cause of pain — and finding the right treatment — can be a difficult journey.
Dr. Lior Baruch, Medical Principal for Cigna Healthcare International Health, answers some commonly asked questions about pain and effective pain management.
Is it true that different people have different pain thresholds?
The most excruciating pain described in the medical literature is a baby delivery. But have you ever seen a man with a cold?
In medicine, patients may be affected differently by similar conditions. The same thing applies to pain. Although the trigger may be the same, patients have different perceptions and reactions. One person may perceive a particular experience as unbearably painful while the other might find it only slightly uncomfortable.
A combination of various factors contributes to an individual's experience of pain. Understanding these differences is essential for effective pain assessment and management and forming the basis for treatment.
Pain is often the primary motive for a patient to seek medical attention, so it’s vital to treat acute pain as soon as possible to prevent chronic issues.
What are the different types of pain, and what causes them?
Pain is classified into three main types: nociceptive, neuropathic, and nociplastic. Determining the type of pain is crucial as it helps medical professionals identify the underlying cause and the right treatment options.
- Nociceptive pain occurs when intact nerve cell endings are stimulated due to tissue injury and inflammation. This type of pain is further divided into somatic pain, which involves receptors in the skin, soft tissue, skeletal muscle and bone, and visceral pain, which involves receptors in internal organs like the kidney and gastrointestinal tract. Somatic pain is usually localised and can be described as sharp, aching, squeezing, stabbing, or throbbing. Visceral pain is often poorly localised and described as dull, crampy, or achy.
- Neuropathic pain is caused by nerve injury resulting from factors such as compression, transection, infiltration, ischemia, or metabolic injury to the nerves. It is commonly characterised by sensations of burning, shooting, electric, or tingling.
People can experience different types of pain at the same time. For example, chronic low back pain and most cancer pain syndromes often have a significant nociceptive aspect as well as neuropathic pain from nerve damage.
- Nociplastic pain can occur without evidence of tissue or nerve damage. It arises from altered nociception, the nervous system’s process of sensing harmful stimuli. The reasons for this type of pain aren’t fully understood.
Are physical and emotional pain linked? If so, how?
Just as physical health affects mental health and vice-versa, both types of pain are associated with alterations in different regions of the brain (the prefrontal cortex and cingulate cortex).
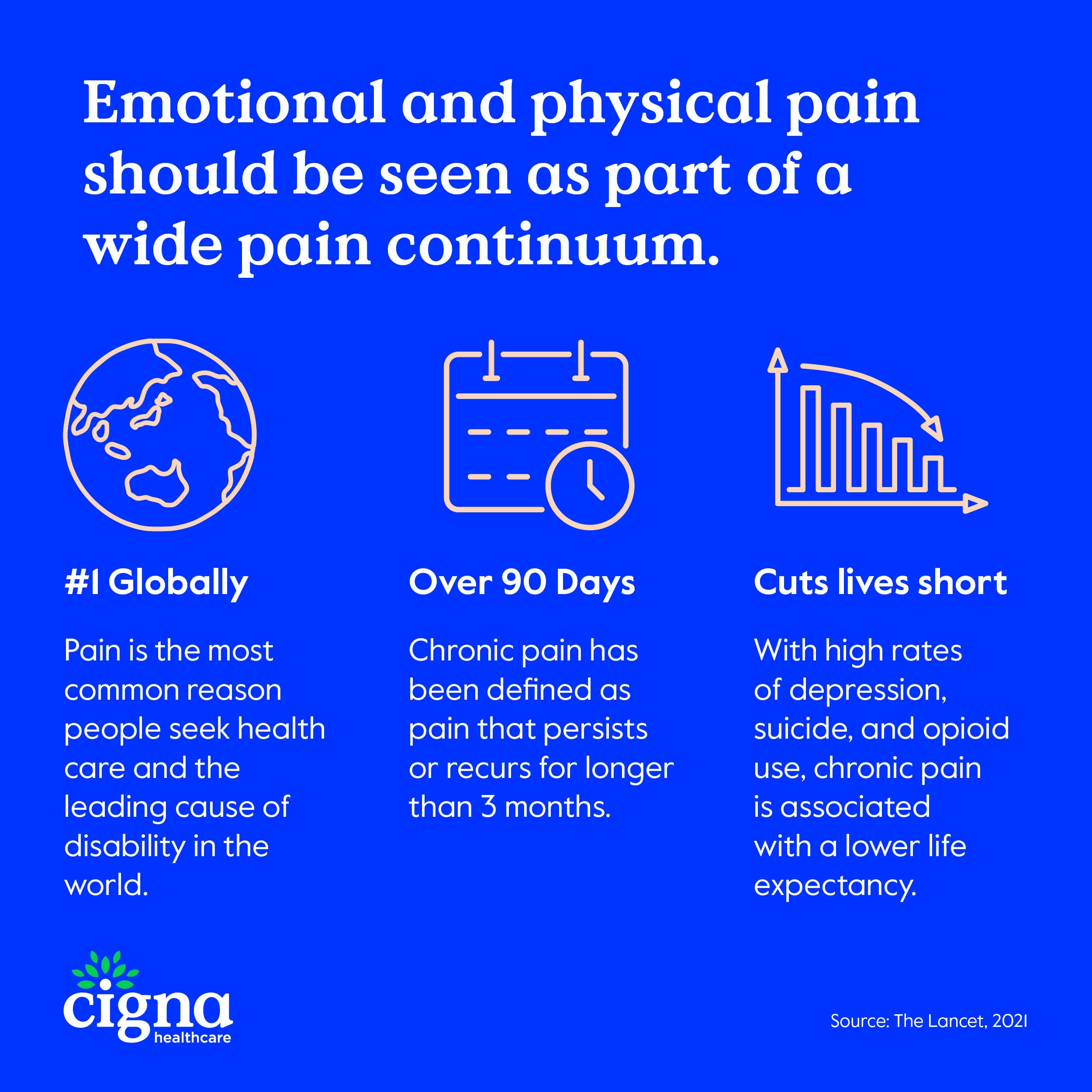
Emotional and physical pain should be seen as part of a wide pain continuum. While some pain is solely physical and some is purely emotional, pain exists on a spectrum in many cases, encompassing both types.
The connection between physical and mental health is complex and not fully understood by experts and researchers. It is known though that there is a reciprocal relationship.
Various factors can contribute to or cause pain. These can build up over time because of physical status, environment, personal memories and experiences, social factors, mental state, and event repetition. Over time, these factors can increase the impact of a person’s pain experience.
As more of these factors build up, people’s pain processes can change, making them more susceptible to developing chronic pain, mental health issues and other factors that can intensify pain.
How often do you encounter patients experiencing chronic pain? What are the common causes?
Chronic pain is one of the most common reasons for patients seeking medical attention. Managing chronic pain requires a multifaceted approach due to its complex nature.
Unresolved, long-lasting disorders such as cancer, rheumatologic conditions, musculoskeletal (MSK) conditions, or back pain can be the sole cause of chronic pain by continuously triggering pain receptors.
This can have knock-on effects. Sleep disturbance is a common consequence of chronic pain, leading to further physical and mental health issues.
Even a mild injury can lead to long-lasting changes in the nervous system, known as sensitization. This can result in persistent pain, even in the absence of triggered pain receptors.
Patients suffering from chronic pain need continuous assessment, education, and support. They also need assistance in establishing expectations for their response to treatment.
Are there scenarios where a patient should in theory experience pain, but it doesn’t, and can it be dangerous?
Yes. A classic one is a silent myocardial infarction (heart attack), which we know is a potential deadly medical emergency, and extremely time-sensitive. However, some patients may experience something called a silent myocardial infarction, which is asymptomatic or demonstrates mild symptoms.
A result of this is patients often not seeking immediate medical treatment. The risk of experiencing a silent myocardial infarction is heightened, for instance, in people with long-term and uncontrolled diabetes. We know diabetes is a significant risk factor for cardiovascular events, but what might be less known is that it also affects pain receptors (afferent neurons) or higher brain areas. And with those areas being compromised, pain triggers don’t kick in as they should.
Thus, diabetes can cause pain not to be perceived, or mildly perceived, even while a dramatic medical emergency might be in course. These patients will not present to the emergency department with a classic excruciating chest pain, yet, they are facing a life-threatening situation.
What difficult decisions do medical professionals have to make when assessing pain management and treatment?
Quality of life, affordability, and medication side effects are key factors to address, as well as mental health impacts. Unfortunately, there’s no silver bullet for every single patient, but it’s important to bring education to the table and empower the patient towards an informed decision.
Understanding the biological, psychological, and social factors behind chronic pain can help alleviate distress and anxiety caused by unexplained symptoms. Patients often have overly severe explanations for their persistent pain, which can exacerbate their experience of pain and lead to unnecessary medical procedures and ineffective treatments.
Rehabilitation-focused pain clinics frequently offer educational group classes for patients experiencing high levels of disability and distress. These programmes aim to address patient concerns about the nature of pain and teach relaxation and reactivation techniques.
Do psychology and cultural attitudes play a major role in how pain is managed and even experienced?
Managing pain is extremely complex. And since every patient is different, cultural aspects are key factors to take into account when trying to solve the puzzle.
The relationship between pain and ethnicity, for example, is influenced by a person's experiences, learning, and cultural background. Erroneous beliefs about pain and disability, reluctance to seek treatment, and failure to take responsibility for treatment outcomes are not exclusive to any particular culture or sub-culture; they are universal obstacles to effective pain management.
Which factors determine the right treatment for pain?
It is important to address specific causes of chronic pain to treat it effectively.
Early treatment of acute pain is highly recommended as it can help limit or prevent sensitization and the experience of pain evolving further. Taking early action can reduce the risk of acute pain progressing into chronic pain. When chronic pain is already established, it becomes necessary to employ multiple treatment methods to address the condition.
The patient's medical status, such as cardiovascular, hepatic, renal, and cognitive issues, can influence the choice of drug used due to potential side effects, drug clearance, and drug-drug interactions.
A holistic approach to care should be adopted, considering biological, social, and psychological factors and using multiple treatment methods. A therapy approach that addresses disturbed sleep, depression, anxiety can also enhance the response to drug and other treatments.
If nonopioid strategies have been maximised and the patient still requires additional relief, opioids may be considered, with options including gradual dose increases, scheduled administration, or intravenous delivery.
Opioids are reserved for patients when other therapies have proven ineffective or are contraindicated, and their risk of non-compliance and misuse is evaluated. When prescribing opioids, the goal is the lowest effective dose for the shortest duration possible, and only if there is measurable improvement in function and quality of life.
Besides medication, which effective methods of pain management exist?
Publicly accessible educational resources and self-management programmes are available online. Selected resources include the following:
- American Chronic Pain Association resource guide and tools
- University of Michigan Fibro Guide self care modules
- US Department of Veterans Affairs Chronic Pain resources
- UK Patient-author guidebook for pain self-management and resources
- US Pain Foundation Patient Resources
- Australian Pain Society Resources
- Working Together With Your Doctor to Manage Your Pain
What are the current priorities in pain research, and what areas require further investigation in the coming years?
Further research is needed to better understand the interactions between biological and psychosocial factors that influence the experience of pain. Identifying individual difference factors and their interactions that contribute to the development and persistence of pain is a top research priority.


